In November 2022, the New Yorker published a devastating report on the state of hospice care in the United States.1 In “How Hospice Became a For-Profit Hustle,” Ava Kofman describes how an end-of-life treatment approach that aims to provide comfort rather than cure can make patients sick. For years, Kofman has been tracking the state of the difficult-to-understand and unevenly regulated hospice industry, interviewing sales representatives, untangling corrupt court cases, and compiling a litany of Medicare frauds—from shell corporations to doctor malpractice to hospices blatantly instructing employees to fabricate patient records. Such schemes are, of course, more than just an orchestrated welfare grift: they ruthlessly exploit people who need healthcare but are struggling to access it. Sometimes they are death sentences.
This violence is usually perpetrated by for-profit hospice companies—a concept that would have been anathema to the group of nurses, doctors, clergy, and activists who first brought hospice care to the United States in the early 1970s as an anti-healthcare establishment movement that wanted to change the way people die. In the intervening half century, hospice, as Kofman summarizes, has mutated “into a twenty-two-billion-dollar juggernaut” that is driven not by ideals but a bottom line: “For-profit providers made up thirty percent of the field at the start of this century. Today, they represent more than seventy percent.”2
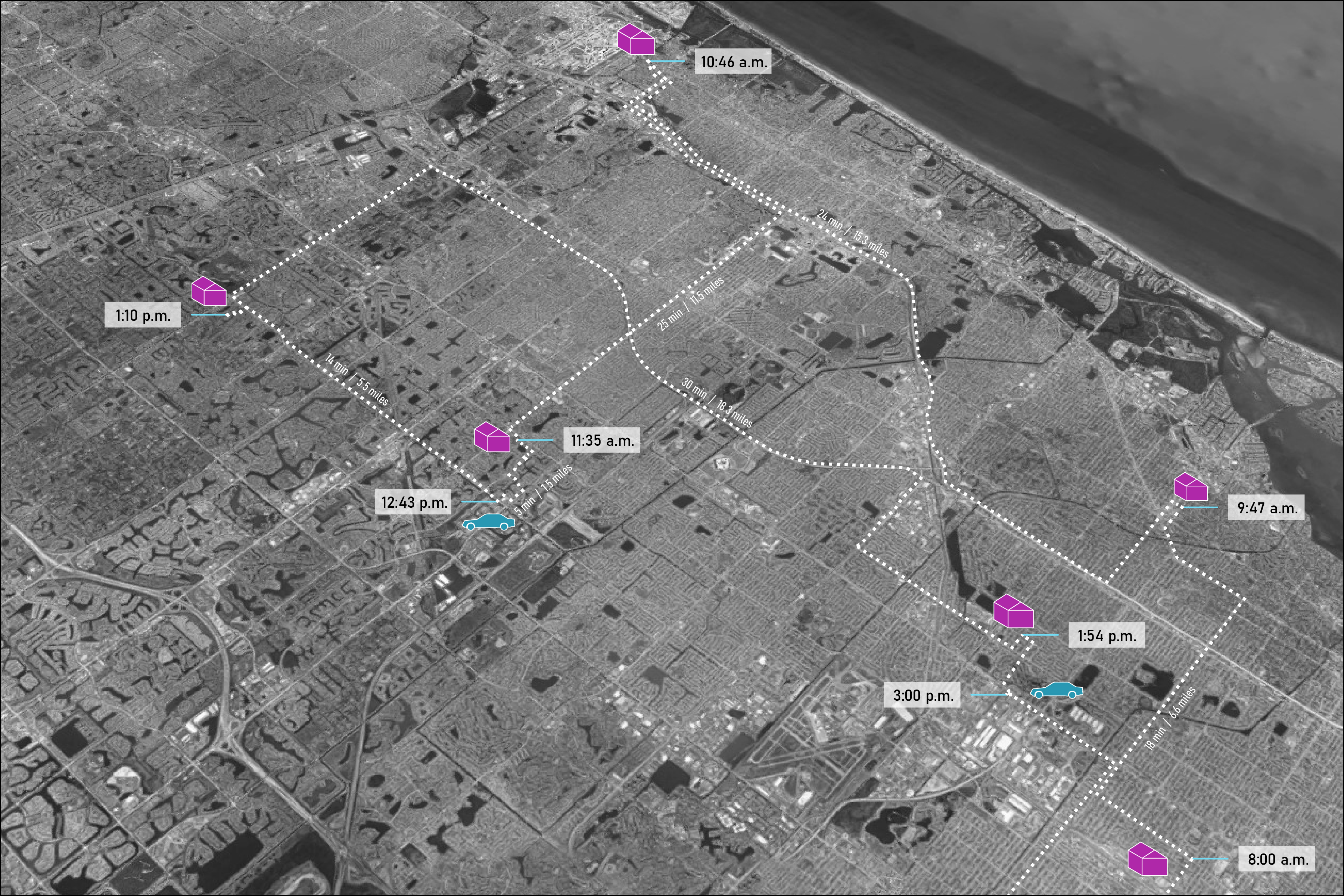
While Kofman’s investigation focuses on for-profit hospices and how they weaponize Medicare against both patients and the state, it also clearly indicates that hospice workers too are a casualty of this system. This problem is far from new.3 Hospice work suffers from the same historical undervaluing that plagues all home health labor, which has long been low-paying, often non-unionized, and relegated to women, working-class immigrants, and people of color.4 It is no coincidence that for-profit hospices primarily operate through home care, only rarely opening inpatient facilities.5 Noticeably, as their market share has grown, so too has the pay gap between home- and facility-based hospice jobs.6 Throughout, hospice care has become less visible to both the public eye and to the state. This loss of spatial legibility, while in no small part driven by patient preference, has enabled corporations to get away with both wage theft and life-threatening malpractice.
As the United States continues to reel from the pandemic-era revelation of just how much hidden care work props up capitalist society, Kofman’s report provokes timely questions.7 What is the relationship between care labor’s devaluation and the shifting spatial conditions in which this labor is performed? And how might the spatialization of hospice care be thought differently so that patients and workers are prioritized over profit? A window might be opened by considering Kofman’s portrait of the present through the lens of a largely forgotten history, one that begins and ends in the quiet suburb of Branford, Connecticut.
61 Burban Drive
Branford’s soft hills and winding, well-maintained roads embody a Connecticut idyll: mostly White, high median income, someone else to mow the lawn. But tucked off Route 1, beyond sight from the road, there is a glitch in the landscape, if you know to look for it. The long, low-slung brick structure at 61 Burban Drive has no inhabitants. Its marshy suburban grounds were, until earlier this year, a favorite daytime walking area for dog owners and retirees—and judging from the constant debris of food, cans, and cigarette butts around nearby benches, a nighttime haunt for another crowd. A Styrofoam plate of cat kibble sat behind one of the columns of the entryway awning. Some days it was full; others, close to empty. It was always soggy.

This is the former Connecticut Hospice, the first purpose-built, freestanding inpatient hospice in the United States. Designed in 1974 and completed in 1980, it embodies the beliefs of a modestly visionary movement that aimed to change how people perceive and experience death. But just as hospice care has transformed from an idealist grassroots practice into a highly codified mode of treatment subject to labor and financial extraction, 61 Burban Drive no longer operates as it used to. The last hospice patient left in 2001; today, the building is being converted into senior housing. Once heralded as an exemplar of innovation that would set the standard for subsequent hospices, its remarkable worker-supportive spatial features—a four-bed patient layout, an attached preschool, and a “scream room”—have been implemented in almost no other facilities.8 For hospice workers who solely make home visits, the favorite model of for-profit companies, such features would be difficult to even imagine. As the hospice movement left its beliefs in the power of considered design and in caring for its own caregivers behind, the Connecticut Hospice’s most ideal-driven architectural gestures became increasingly less influential—and in some cases, like the building itself, even obsolete.9 But this disposition need not be a permanent one.
Hospice as spatial practice
The US government defines hospice as end-of-life treatment that “provides comprehensive comfort care as well as support for the family” while “attempts to cure the person’s illness are stopped.”10 To qualify for hospice, a patient must have received a terminal diagnosis and a prognosis of less than six months to live. As the government considers hospice “an approach to care,” it further defines it as “not tied to a specific place.”11 It can occur in a patient’s home, a dedicated facility, a nursing home or other long-term, residential care institution, or a hospital.
While this placeless conception of hospice is now widely accepted and practiced, the modern hospice movement was inspired by and named after a historical building typology—the hospice of the early Christian era—and conceived as an inherently spatial practice.12 Specifically, hospice was formulated, in the 1950s and ’60s, as a care philosophy that offered an alternative to dying in a hospital, an experience that was becoming increasingly common and increasingly traumatic. Average life expectancy in the United States had risen dramatically in the first half of the twentieth century, from fifty to sixty-eight years, and, as a corollary, death from incurable chronic illness became more prevalent.13 The medical establishment, however, did not react in step. Rather than develop new approaches for handling the painful, often slow declines that such diagnoses harbingered, hospitals—sites of both exploding medical knowledge and an arguably naïve postwar technological optimism—vigorously attempted to cure patients until almost the moment of death.14 As a result, pain control and symptom management were unevenly administered during a patient’s final weeks and days. (This was especially true for women and people of color, whose expressions of discomfort were more likely to be downplayed by doctors.)15 Caretakers, friends, and families of the dying, too, experienced increasing trauma as they watched this suffering unfold in spaces that were perceived as “unfeeling, uncaring, and impersonal.”16
In an act of protest against the awful hospital deaths she witnessed, Cicely Saunders, a British nurse, social worker, and eventual doctor, undertook pioneering research on end-of-life care and pain control in the 1950s with a mind toward reform. By the early 1960s, she was convinced that for such reform to be deep and impactful, it could not occur within the space of the hospital, and so she began planning the first contemporary hospice. It would be a purpose-built, freestanding inpatient facility in London, only for terminally ill patients; it would not attempt to cure, nor would it wrap patients in the band-aids of avoidance and denial so overused by hospital doctors.17 Instead, its carefully designed spaces would offer workers and families a setting of respite and calm, which would provide patients with community, attention, comfort, and acknowledgment, as well as a social support network of loved ones and caretakers, with a stated goal to treat their “total pain.”18
St. Christopher’s Hospice, designed by the architect Peter Smith in close collaboration with Saunders, opened in South London in 1967 as the first purpose-built space for modern hospice care.19 The inclusion of care workers within the framework of treatment—a radical notion within the medical establishment at the time, yet one that the US healthcare labor movement was also starting to seize on—was crucial to Saunders.20 If care workers were not themselves valued and provided for, how could they possibly be present for others?
In 1963, Saunders took her research on a lecture tour in the United States, trying to plant the seeds of hospice. One took root in Connecticut. Among the audience members at her talks at the Yale School of Medicine on April 2 and 3 was Florence S. Wald, then the dean of the Yale School of Nursing.21 Saunders’s lecture opened a door that would lead Wald to resign her deanship in 1967 and dedicate herself to bringing hospice care to the United States.22 Her husband, Henry Wald, was similarly convinced. He closed his engineering practice in the late 1960s and joined Florence’s endeavor, heading back to school for a master’s in architecture, with the intention of laying the groundwork for an inpatient facility.23 As only one other hospice (St. Christopher’s) had ever been designed to serve as a precedent, the Walds felt it was crucial to undertake careful study of the potential spatial, technical, and programmatic aspects of a dedicated hospice building.
With guidance and encouragement from Saunders, the Walds gathered a group of New Haven–based nurses, doctors, clergy, and laypeople to form the first hospice organization in the United States: Hospice, Inc., incorporated in 1971.24 Hospice, Inc. would offer both inpatient and home care, the latter of which could be launched relatively quickly and begin to bring in funds.25 Planning and design of the inpatient facility began as soon as the organization was formed.
“The architectural setting is a major contributor.”
A 1972 proposal for the site selection and schematic design of the inpatient facility provides a look into the romantic, somewhat vague, but passionate approach of the early Hospice, Inc. days. This attitude would shape the design of the Connecticut Hospice.26 According to the Walds and the organization’s other founders, a specific, carefully planned building was needed to carry out the goals of hospice:
The plans for the building and site are predicated on the hypothesis that the services can best be provided by a system in which the architectural setting is a major contributor... The structure should convey the philosophy and goals of the Hospice program that is, to maximize the quality of life of patients, to serve the family as well as the member who is ill, and to know what staff needs to function well and provide for those needs.27
Like Saunders, the Walds considered the patient’s support system, including their paid care workers, an integral part of hospice:
We recognize that those who help the terminally ill, whether family, friend or worker expend tremendous energy which needs replenishment. Therefore the quality of the ongoing relations of one worker to another, especially in the openness and concern for one another, is essential to sustain the Hospice community. In this facility we will question certain values. For example how important is privacy? What kinds of people and skills help?28
The stated intent to “question certain values” through the facility’s design would eventually lead Hospice to hire Lo-Yi Chan, a cofounder of the New York–based firm Prentice & Chan, Ohlhausen, as the building’s architect. A young yet accomplished practitioner, Chan had never designed a healthcare facility. This very lack of experience, however, was “a major reason why he was hired,” as the founders of Hospice, Inc. expressly did not want to work with an architect with preconceived notions of what a healthcare space should be.29 Upon receiving the commission, Chan traveled to London in 1973, observing St. Christopher’s use patterns and interviewing patients.30 Like Saunders and Wald, he began to draw a distinction between what hospital architecture prioritized—efficiency, technology—and what the ideals of hospice care demanded instead.
In close consultation with the Hospice, Inc. team, and with the Walds in particular, Chan completed the design for the Connecticut Hospice in July 1974.31 The facility was built over the next six years, and on July 7, 1980 received its first patient.32
Foregrounding care worker needs
The Connecticut Hospice was a modest two-story redbrick building with generous glazing, encompassing approximately 42,000 square feet.33 By multiple accounts, it was unimposing, inviting, and fit seamlessly into the landscape, more like a small-town civic building than a mega-hospital.34 Its interior was organized around a long corridor: administrative spaces on one side, patient spaces zigzagging along the other. Within the corridor itself were two freestanding nursing stations that served as the primary nodes connecting patients and staff. The patient spaces were carefully perforated and layered in plan to encourage movement and create opportunities for community, connection, and a sense of life: first, public common rooms, dining areas, and a chapel; next, patient rooms; then a shared interior greenhouse hallway; and, finally, two communal outdoor terraces. A partial mezzanine level, almost entirely programmed for staff use, sat atop the corridor and first-floor administrative spaces.
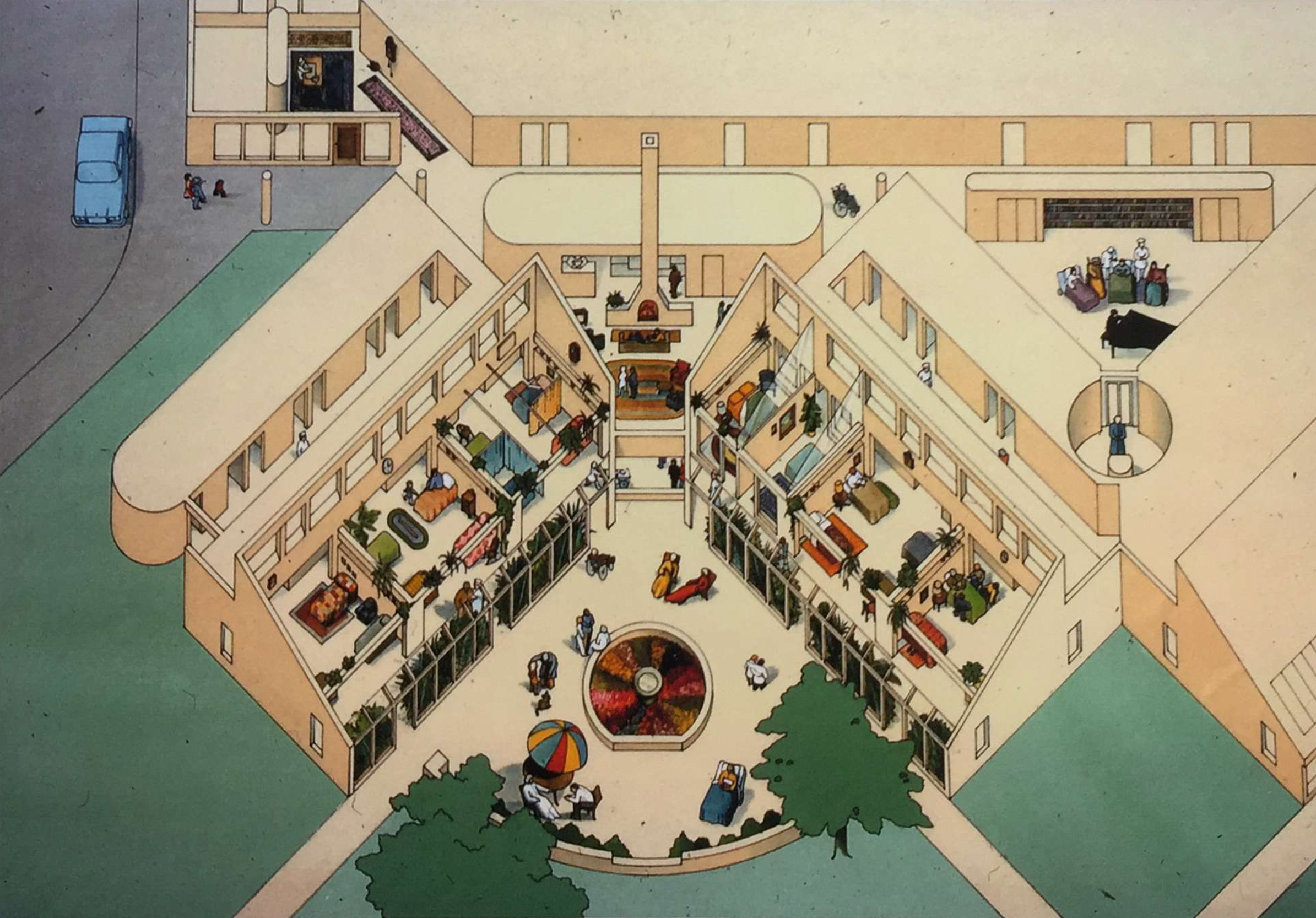
Three features are especially key to considering the building’s attitude toward care workers. The first is its bed configuration: out of its forty-four total beds, just four were in single rooms (usually reserved for special cases, such as patients with infectious diseases). The remaining forty were distributed across ten four-bed rooms. John D. Thompson and Grace Goldin note in The Hospital, their canonical history of the typology, that “no hospital problem has generated more heat in modern times than the issue of privacy, particularly in the United States,” and this would eventually become true for hospices as well.35 But among the founders of the modern hospice movement, it was an axiom that private rooms isolated patients and drove them further into loneliness. Crucially, it was also easier for nursing staff to monitor and care for patients in clusters than in individual rooms. As Dr. Sylvia Lack, Hospice, Inc.'s first home-care director, and Chan explained to a journalist in 1976, the configuration was developed with the well-being of not only patients but also care workers in mind. The low partitions Chan placed between rooms allowed staff to easily see patients from wherever they were, and his design of the rooms themselves allowed patients and their families to assist staff in checking in on other patients, contributing to the emotional labor of routine caretaking.36 Former Connecticut Hospice workers recall that the relationships between patients in these shared spaces both enriched and relieved their responsibilities.37

A preschool was another key spatial and programmatic element of the Connecticut Hospice that supported the imperative “to know what staff needs to function well and provide for those needs.”38 Incorporated into the hospice in early 1982, the Charlie Mills Preschool ran a ten-month, five-day-a-week school year for three- and four-year-olds.39 One of the only such programs ever to exist at a hospice in the United States, and certainly the first of its kind, it thrived for at least six years, usually hosting around twenty-five children at a time. Attendees included children of staff as well as local residents. And while the preschool’s presence ended up providing, per multiple accounts, significant benefits to patients, it was originally conceived for the benefit of children and staff.40 Dawn Ralston, whose mother, Dawn D’Amato, was a nurse’s aide at Connecticut Hospice from 1980 to 1984, shared deeply fond memories of attending the preschool in a 2020 interview and said that it “absolutely” influenced her own decision to work in hospice as an adult.41 In the same conversation, D’Amato noted that the facility lessened her load as a parent.42

Among the design gestures that aimed to support both laborer and patient, the most explicitly worker-oriented feature in the building was also its most architecturally experimental. The “scream room,” tucked away at the northern end of the mezzanine level, was an ellipsoid, soundproof, fully carpeted volume of 114 square feet.43 A stepped platform, carpeted in the same beige as the walls and floor, rose toward the ceiling, where a large skylight swooped down to meet it. There were no other light sources, electric or otherwise.44 The room’s furniture consisted of a single bean bag.45 This otherworldly interior—more akin to a set piece for a Pierre Cardin ad than to an institutional break room—was Chan’s “idea of architectural therapy”: “a nonobjective space for ventilation of emotions and replenishment of energy” that would “cool the psyche.”46 During a particularly difficult shift, a nurse could leave the floor and head upstairs to yell out their frustration, cry, or simply relax in the swaddled room, whose rounded shape made it, according to Chan, “almost womblike.”47
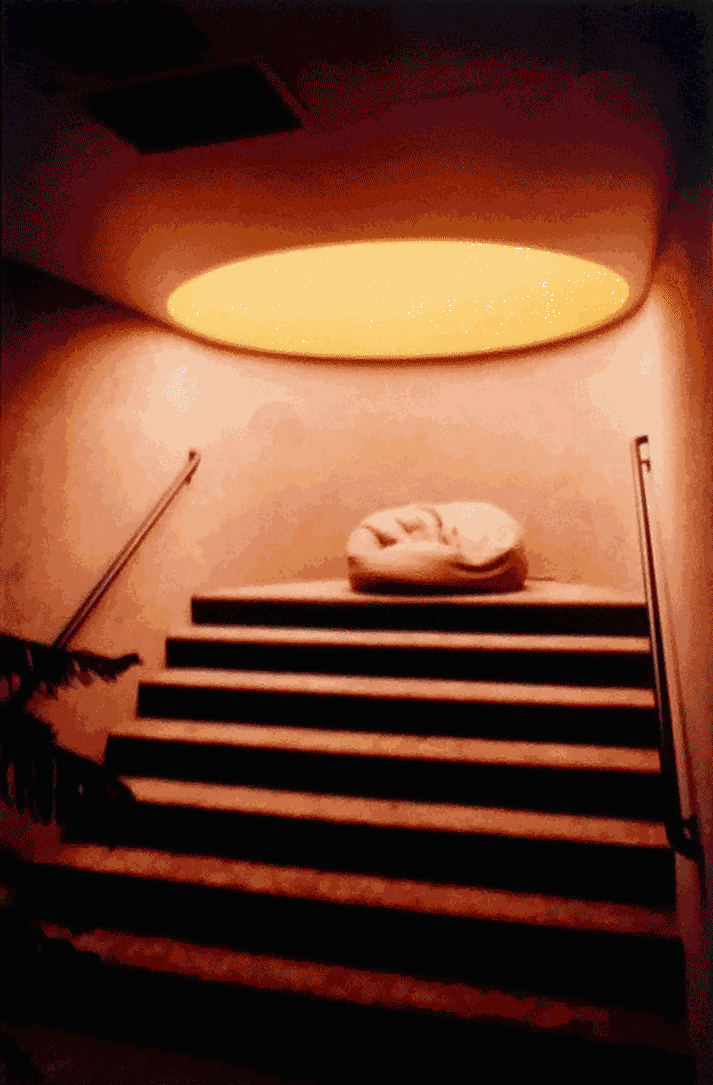
Its genesis is as personal as the room is unusual. In the 1970s, Chan had a neighbor in primal therapy, the psychotherapeutic method developed by Arthur Janov that directs patients to release their trauma by vocalizing it. He recalls hearing this neighbor making guttural cries—and though this worried Chan at first, other neighbors explained that it was in fact a healing practice.48 The scream room was intended to provide a space for this same type of catharsis, and, in doing so, to address the hospice movement’s stated aim to take care of professional caregivers.49 It was without precedent in healthcare architecture.50 In recent interviews, four former Connecticut Hospice workers—D’Amato, Deborah Gleason St. John, Genevieve O’Connell, and Dianne Puzycki—all shared unanimously positive impressions of the scream room and cited it as a necessary part of any hospice facility.51 Puzycki remembered how calming it was, and the advantage of it being hidden away from the main circulation paths, “so that nobody knew you were having a hard time.”52 “Everybody loved that room,” said O’Connell. “Sometimes, especially after a difficult conversation with a patient’s family, you just needed to go cry, or go look up at the stars.”53
The crush of the market
That was then; this is now. In the decades following the Connecticut Hospice’s opening, none of its worker-oriented spatial features—the four-bed rooms, the integrated preschool, the scream room—were widely copied.54 Instead, as the hospice movement grew in both scope and scale, providers were faced with increasing regulatory considerations, rising costs, and changing consumer preferences that reflected a nationwide trend toward the commercialization of healthcare spaces. As a result, hospice soon began to be shaped less by ideals than by the immiserating pressures of market capitalism.55 As Emily K. Abel diagnosed in a perceptive 1986 article,
The early leaders of the hospice movement shared a number of attitudes with the founders of the alternative institutions of the 1960s and early 1970s: nostalgia for simple, old fashioned ways, dissatisfaction with bureaucratic and authoritarian institutions, faith in the power of nature, a determination to avoid domination by experts, and a desire to improve the quality of personal relationships. However, as hospices have become better established, they gradually have been incorporated into the dominant health care system and have lost their uniqueness.56
Many factors contributed to this integration of hospice care into the mainstream, but perhaps the most consequential was Congress’s passing of the 1982 Tax Equity and Fiscal Responsibility Act, which created a provisional Medicare hospice benefit.57 Hospice advocates generally supported the benefit, as it promised to widely extend the promises of hospice that they so firmly believed in. The Reagan administration’s reason for rubber-stamping it was perhaps less altruistic: After almost ten years of federal trials and studies, the Medicare budget office had reached the conclusion that adding a hospice benefit would be kind to their bottom line.58 In 1986, the Medicare benefit was made permanent, and, in the mid-1990s, during the height of the AIDS crisis, hospice also became a benefit of Medicaid.59 The availability of federal funding for both institutions and patients has dramatically shaped the succeeding course of hospice. Though it has absolutely expanded care access, this funding has also been exploited by the arrival of for-profit institutions.60
The industry’s own perspective on hospice inpatient environments has also changed, and research from the past decade suggests a different hierarchy of organizational goals than those embodied in the design of the Connecticut Hospice. The individual patient and their privacy are routinely identified as top priorities; workers are discussed with less frequency. In 2016, the first-ever post-occupancy evaluation tool was designed for hospice environments; out of the eleven therapeutic goals it determined should be used to evaluate building performance, eight concern the autonomous patient. One each addresses social needs, family, and staff.61 Similarly, in the Cornell-produced handbook Designing End-of-Life Care Settings to Enhance Quality of Life (2018), design considerations are almost entirely focused on patient needs.62 Again, privacy is paramount: “The ideal is to provide single occupancy rooms with closeable doors to give each resident and his or her family full control of privacy.”63 Here, at least, there is the recommendation for a staff break room. Within is a TV, rather than a skylight through which to gaze at Orion on a breathless winter night.
Spatial imbrications, new horizons
Shifting institutional priorities eventually led to the abandonment of 61 Burban Drive. In 1999, after years of considering such a move, the board of the Connecticut Hospice—which no longer included any of its original members—announced it would be selling the Chan-designed facility it had occupied for nineteen years and moving into a significantly larger former corporate headquarters on the waterfront a few miles away.64 By 2001, 61 Burban Drive had been sold to the Benedictines of Jesus Crucified, a Roman Catholic order that gives vocations to women with physical disabilities who might otherwise be rejected from religious life.65 During their ownership, it became the Monastery of the Glorious Cross and underwent exterior and interior renovations. A bell tower was added to one of the former patient terraces; bathrooms were updated; the four-bed wards were chopped up into smaller cells.66
The nuns lasted not quite as long as the terminally ill. In 2018, 61 Burban Drive was once again on the market. “Perfect for school or non-profit,” the listing said.67 Three years later—in the summer of 2021—the building was sold to a private real estate developer.68 It remained untouched until this past winter, when a thorough interior demolition commenced: the first stage in a plan to convert the former hospice into “The Views,” a fifty-nine-unit senior housing complex.69 As winter gave way to spring, more and more of the building’s memory was discarded into dumpsters. Now little more than the structure and façade remains.
What is there to learn from the annals of this remarkable building soon to embark on its third incarnation—in which it will once again house people nearer to life’s end than its beginning? The staggering breadth of exploitation and suffering catalogued by Kofman in her investigation for the New Yorker forestalls any inclination to look for a singular solution to the hospice crisis; it is tendriled and ever-shifting, like capitalism itself. Architecture cannot inhibit the market (usually it does the opposite). But for a moment in history, the Connecticut Hospice sincerely attempted to spatially manifest its ambition to yoke the well-being of patients to the well-being of staff, weaving together the fates of two populations commonly cast aside by the state and by capital as outside the realm of production and therefore without value, yet still ripe for extraction. There may yet be a seed to find, a vine to plant, in furtherance of this radical vision of hospice that foregrounds labor as itself deserving of architectural care.70

-
Ava Kofman, “How Hospice Became a For-Profit Hustle,” New Yorker, November 28, 2022, link. Kofman’s article has already spurred reform in how the Centers for Medicare and Medicaid Services oversee hospice providers and prompted investigations into multiple providers she discussed. See “Ava Kofman Wins Hillman Prize for ‘Endgame,’” ProPublica, April 25, 2023, link. ↩
-
Kofman, “How Hospice Became a For-Profit Hustle.” ↩
-
Paula Span, “Short on Staff, Some Hospices Ask New Patients to Wait,” New York Times, October 16, 2021, link. ↩
-
For an extensive history of why hospice and other home healthcare workers are simultaneously so in-demand and so poorly paid, see Eileen Boris and Jennifer Klein, Caring for America: Home Health Workers in the Shadow of the Welfare State (New York: Oxford University Press, 2012). Boris and Klein marshal significant historical evidence to show that the welfare state’s long-term reliance on private entities to mediate between the government and care workers has kept these workers outside the realm of labor protection and public visibility. A shorter and more contemporary discussion of the same issue can be found in “Who Cares for the Caregivers?” n+1 39 (Winter 2021): 1–8. ↩
-
Ira Byock and Eric Walsh, “Hopewell Hospice Has Closed. You Should Care About That,” STAT, November 19, 2019, link. ↩
-
In 2000, the median hourly wage for home health aides—including those working in hospice—was $8.71, barely below the $8.89 made by nursing assistants, who perform very similar work to home health aides but are typically stationed in facilities. In 2022, home health aides were making a median of $14.51, about 76 percent more than in 2000, whereas the wage for nursing assistants had increased by almost 100 percent, to $17.19 an hour. Bureau of Labor Statistics, “Occupational Employment and Wages, 2000” (Washington, DC: U.S. Department of Labor, 2002), 3, 12; “May 2022 National Occupational and Wage Statistics,” U.S. Bureau of Labor Statistics, link. Despite its higher median pay, nursing assistant labor is of course still deeply undervalued, precarious, and frequently exploitative. For a visceral account of one assistant’s attempt to organize for better working conditions within their nursing home facility, see Jomo, “Caring: A Labor of Stolen Time: Pages from a CNA’s Notebook,” Lies: A Journal of Materialist Feminism 1 (2012): 69–100. Thanks to Jack Rusk for bringing this text to my attention. ↩
-
Nancy Fraser offers a clear if simplified framing of capitalism’s reliance on invisible labor, and how race and gender are weaponized by capital to this end, in “Behind Marx’s Hidden Abode: For an Expanded Conception of Capitalism,” New Left Review 86 (March/April 2014): 55–72. ↩
-
The founders of the Connecticut Hospice, too, were explicit in their hope that the building would “serve as a model for others.” Hospice, Inc., “Proposal: Site Selection and Schematic Design” undated (ca. 1972), 8, box 1, folder 3, Florence and Henry Wald Papers, Manuscripts and Archives, Yale University Library. ↩
-
I do not mean to claim that no hospices put stock in the role of architectural design, but within the United States it is now rare to find a hospice building whose design does much but check the standard boxes of efficient circulation, outdoor views for each room, and easy-to-clean materials. One exception that unfortunately closed in 2018 was San Francisco’s Zen Hospice Project’s Guest House, an adapted Victorian town house that served the dying for almost thirty years, having opened around the peak of the AIDS crisis. Former nursing assistant Celeyce Matthews recalls her experience as a staff member there in “Dying Days at the Guest House,” Zen Caregiving Project, December 23, 2019, zencaregiving.org/2019/12/dying-days-at-the-guest-house/. Additionally, the UK and Japan have more robust and experimental hospice-design traditions than the United States. See Stephen Verderber and Ben J. Refuerzo, Innovations in Hospice Architecture (Abingdon, UK: Taylor and Francis, 2006), 41–57. ↩
-
“Understanding Hospice Care,” National Institute on Aging, link. ↩
-
“Understanding Hospice Care.” ↩
-
The word hospice was first used to describe a category of buildings that were “essentially inns for pilgrims,” constructed along popular Christian pilgrimage routes from the early centuries of the first millennium CE into the Middle Ages. Hospices were typically part of monastic complexes, within which they were spatially and programmatically specific. Travelers could stay for a night or for a month, recuperating until they were ready to resume their journey, and would receive both sustenance and medical care from the resident monks. John D. Thompson and Grace Goldin, The Hospital: A Social and Architectural History (New Haven, CT: Yale University Press, 1975), 6–8. See also Sarah McGann, The Production of Hospice Space: Conceptualising the Space of Caring and Dying (London: Routledge, 2013). ↩
-
Janet Sopcheck, “Social, Economic, and Political Issues Affecting End-of-Life Care,” Policy, Politics & Nursing Practice 17, no. 1 (2016): 33. ↩
-
Edward H. Rynearson, “You Are Standing at the Bedside of a Patient Dying of Untreatable Cancer,” CA: A Cancer Journal for Clinicians 9, no. 3 (May/June 1959): 85. ↩
-
Charles Rosenberg, The Care of Strangers: The Rise of America’s Hospital System (New York: Basic Books, 1987), 6. ↩
-
On caretaker trauma, see, for example, chapter 5 of Emily K. Abel, The Inevitable Hour: A History of Caring for Dying Patients in America (Baltimore: Johns Hopkins University Press, 2013), which recounts Dorothy Smith Dushkin’s experience of her daughter Amanda’s long and difficult hospital death in 1962. For a note on how the functional, rationalist character of the modernist hospital contributed to said trauma, see David Charles Sloane, “Scientific Paragon to Hospital Mall: The Evolving Design of the Hospital, 1885–1994,” Journal of Architectural Education 48, no. 2 (November 1994): 88. ↩
-
In addition to their unfamiliarity with palliative care techniques, doctors at this time were rarely trained in end-of-life conversations with patients, resulting in “a death-denying culture” within hospitals; see David Clark, “Palliative Care History: A Ritual Process?” European Journal of Palliative Care 7, no. 2 (2000): 50. Current research indicates that physician education is still seriously lacking in this regard. A 2003 study found that less than 18 percent of medical students and residents reported receiving formal training in end-of-life care; this percentage was even lower in a similar 2016 study, in which just 11.9 percent of residents said they had received in-class end-of-life care education. What education does take place is not distributed evenly among patients. A 2015 report found that minority patients with histories of economic and educational disadvantage are less likely to have end-of-life conversations than other patients and are correspondingly more likely to die in unsatisfactory situations. Ryan Sutherland, “Dying Well-Informed: The Need for Better Clinical Education Surrounding Facilitating End-of-Life Conversations,” Yale Journal of Biology and Medicine 92 (2019): 758–759. ↩
-
Verderber and Refuerzo, Innovations in Hospice Architecture, 15; “Dame Cicely Saunders: Her Life and Work,” St. Christopher’s Hospice, link; Mary Baines, “Pioneering Days of Palliative Care,” European Journal of Palliative Care 18, no. 5 (2011): 223–227. ↩
-
Avnita Amin, “St. Christopher’s Hospice: A Space for the Dying,” Archives of Dame Cicely Saunders (1918–2005) (blog), December 14, 2015, link. ↩
-
The US healthcare labor movement was beginning to seriously pick up in the late 1960s, around this very same time. See Edmund R. Becker, Frank A. Sloan, and Bruce Steinwald, “Union Activity in Hospitals: Past, Present, and Future,” Health Care Financial Review 3, no. 4 (June 1982): 1–13. The movement’s connection between patient and worker well-being especially comes through in strike language; see, for example, Boris and Klein’s account of the New York–based Campaign for Justice for Home Care Workers in 1987, which used the slogan “We Care for the Most Important People in Your Life” (Caring for America, 179), or, more recently, signs held at the 2023 nurses’ strike at Mount Sinai and Montefiore hospitals in New York emblazoned with phrases like “On Strike for Better Patient Care” and “Fair Contract for Patients and Nurses.” Chris Isidore, “Health Care Is in Crisis. New York’s Nurse Strike Is Just the Latest Sign,” CNN, January 11, 2023, link. ↩
-
For the lecture dates, see Kai Chun Tang, “StoryMap: Cicely Saunders’ USA Tour, 1963,” Archives of Dame Cicely Saunders (1918–2005), September 14, 2015, link. For a detailed account of the two talks, see David Clark, To Comfort Always: A History of Palliative Medicine Since the Nineteenth Century (Oxford: Oxford University Press, 2016), 98. ↩
-
Emily K. Abel, Prelude to Hospice: Listening to Dying Patients and Their Families (New Brunswick, NJ: Rutgers University Press, 2018), 16. Many sources misdate Wald’s resignation from Yale as 1965 or 1966; however, 1967 is confirmed in numerous archival documents in the Wald Papers. ↩
-
In 1971, Henry Wald graduated from the Columbia University Graduate School of Architecture and Planning with the thesis A Hospice for Terminally Ill Patients. See Abel, Prelude to Hospice, 14. ↩
-
Hospice, Inc., “Proposal,” 9. ↩
-
Hospice, Inc., “Proposal,” 4. ↩
-
The proposal—a carefully formatted typescript in a simple two-cover binding—occasionally employs strange turns of phrase or omits punctuation. These idiosyncrasies have been preserved in the succeeding transcriptions. ↩
-
Hospice, Inc., “Proposal,” 1. ↩
-
Hospice, Inc., “Proposal,” 5. ↩
-
Paul Goldberger, “Architecture: Connecticut Hospice,” New York Times, December 4, 1980, C20. See also Joan Kron, “Designing a Better Place to Die,” New York, March 1, 1976, 47. ↩
-
Further, Kron wrote of the visit, “Chan came away from St. Christopher’s as most visitors do—evangelized.” Kron, “Designing a Better Place to Die,” 47; Lo-Yi Chan, “Hospice: A New Building Type to Comfort the Dying,” AIA Journal 65, no. 12 (December 1976): 44–45. ↩
-
For the dating of Chan’s design, see Prentice & Chan, Ohlhausen, “Hospice: Site Plan,” “Hospice: Plans,” “Hospice: Elevations,” architectural drawings, July 31, 1974, box 1, folder 3, Wald Papers. According to Chan, the building’s form and gestures were original to him rather than to Henry Wald’s thesis; when asked how much influence the thesis had, Chan replied that he “would characterize [it] as important, but at the same time, not important... it set out the technical basis... but it didn’t specify in any way the shape of the building or the thinking behind the building.” Lo-Yi Chan, interview with the author, January 8, 2021. However, the Wald Papers suggest that the Walds exerted heavy—one might even say overbearing and, at times, jealous—involvement later in the design process. See, for example, “Memorandum: Conference with Lo-Yi Chan, Henry Wald and Florence Wald,” received July 16, 1974, box 1, folder 2, Wald Papers, and letter from Lo-Yi Chan to Henry Wald, December 4, 1975, box 3, folder 24, Wald Papers. In the former, the Walds present a long and granular list of design criticism to Chan, on everything ranging from storage placement to corridor length to what kind of view patients should have of the kitchen; in the latter, Chan seems to be responding to a letter from Henry that accused Chan of taking too much credit for the design of the Connecticut Hospice. ↩
-
“Hospice Groundbreaking,” printed event pamphlet, November 20, 1977, box 1, folder 5, Wald Papers; “The Region: Connecticut Hospice for Terminally Ill,” New York Times, June 30, 1980, B4. On the six-year span between design completion and the facility’s opening: a slew of setbacks interrupted the building process—many financial, some organizational, others personal. Most notable was Florence Wald’s forced resignation from the Hospice, Inc., board, due to complaints of micromanagement from other team members. The setbacks are detailed in the Wald Papers; on Wald’s resignation, see Emily K. Abel, Living in Death’s Shadow: Family Experiences of Terminal Care and Irreplaceable Loss (Baltimore: Johns Hopkins University Press, 2017), 123. ↩
-
“The Region: Connecticut Hospice for Terminally Ill.” ↩
-
Paul Goldberger, for example, wrote just after the building opened that “from the outside, the Connecticut Hospice could be a suburban school—the mix of red brick, wood and glass in a low structure calls to mind many a small-town elementary school… [it] is without pretence. It is comfortable, and thoughtful, but above all, its architecture is honest in its intentions.” See Goldberger, “Architecture: Connecticut Hospice.” See also Verderber and Refuerzo, Innovations in Hospice Architecture, 16. ↩
-
Thompson and Goldin, The Hospital, 207. ↩
-
Chan, “Hospice,” 44; Kron, “Designing a Better Place to Die,” 48. ↩
-
In an interview, former Connecticut Hospice nurse Dianne Puzycki recalled a particularly “helpful” and “wonderful” example of what shared rooms could yield. A patient in a shared room began actively dying and was particularly anxious, Puzycki remembered, crying out continuously in fear. One of her roommates was a patient with ALS who the staff believed had lost her ability to talk. Soon after the dying patient started to express her fear, however, the patient with ALS began to speak words of comfort to her. Dianne Puzycki, phone interview with the author and Genevieve O’Connell, December 24, 2020. ↩
-
Hospice, Inc., “Proposal,” 4. ↩
-
Robert E. Tomasson, “A Happy Exchange at Hospice,” New York Times, January 9, 1983, CN2. ↩
-
Tomasson, “A Happy Exchange at Hospice,” CN2. ↩
-
Dawn Ralston, interview with the author and Dawn D’Amato, December 23, 2020. ↩
-
Dawn D’Amato, interview with the author and Dawn Ralston, December 23, 2020. ↩
-
The room’s location is not marked on the original building plans; this information is from Genevieve O’Connell and Dianne Puzycki, phone interview with the author, December 24, 2020. For the square footage, see Deborah Allen Carey, Hospice Inpatient Environments: Compendium and Guidelines (New York: Van Nostrand Reinhold, 1986), 66. This area is much smaller than Chan had originally hoped: numerous planning documents in the Wald Papers show it was intended to be 400 square feet. ↩
-
Kron, “Designing a Better Place to Die,” 49. ↩
-
Kron discusses this furniture situation in her 1976 article, saying that “the carpet-lined retreat will have no furniture except, perhaps, bean bags” (Kron, “Designing a Better Place to Die,” 49), but I was skeptical that it had in fact been implemented. However, three staff members who worked at Connecticut Hospice in the 1980s and 1990s not only confirmed its implementation but said that the bean bag was never swapped out in favor of something more practical. O’Connell and Puzycki, phone interview with the author, December 24, 2020; D’Amato, phone interview with the author and Dawn Ralston, December 23, 2020. ↩
-
Chan, interview with the author, January 8, 2021; Chan, “Hospice,” 45; Kron, “Designing a Better Place to Die,” 49. ↩
-
Dee Wedemeyer, “Hospitals Designed for the Dying,” New York Times, May 28, 1978, R4. Both this commentary and the design itself reveal how even the spatialization of care for care workers is gendered here. It is not enough that the laboring female body is employed to reproduce others, it must also reproduce itself. ↩
-
Chan, interview with the author, January 8, 2021. ↩
-
Kron, “Designing a Better Place to Die,” 49. ↩
-
In fact, Chan states that it was without precedent of any kind—that he had never been in a room like this, and that he essentially created it whole cloth, with no explicit input from the Hospice, Inc. founders, who approved of his design on first viewing. Chan, interview with the author, January 6, 2021. ↩
-
D’Amato, interview with the author and Dawn Ralston, December 23, 2020; Deborah Gleason St. John, interview with the author, January 6, 2021; O’Connell and Puzycki, phone interview with the author, December 24, 2020. ↩
-
As indicated by Puzycki, the privacy of the scream room appears to have been fundamental to it being a restorative space, a place where staff could reclaim a sense of a bounded self after particularly difficult encounters in which they felt engulfed, even erased, by their encounters with patients. Puzycki, phone interview with the author and Genevieve O’Connell, December 24, 2020. ↩
-
O’Connell, phone interview with the author and Dianne Puzycki, December 24, 2020. ↩
-
Carey, Hospice Inpatient Environments, 33–35, 65, 184–185, 217, 238–239; see also individual compendium entries for each of the forty-eight facilities. ↩
-
On the commercialization of healthcare spaces in the US, see, for example, Sloane, “Scientific Paragon to Hospital Mall,” 82–98. ↩
-
Emily K. Abel, “The Hospice Movement: Institutionalizing Innovation,” International Journal of Health Services 16, no. 1 (1986): 71. ↩
-
Abel, The Inevitable Hour, 169. ↩
-
Estimates were that this extension would allow for $1,100 less to be spent per patient than the same pre-death care would cost in a hospital—yielding an estimated $48 million in savings in just the first three years. Feather Ann Davis, “Special Report: Medicare Hospice Benefit: Early Program Experiences,” Health Care Financing Review 9, no. 4 (Summer 1988): 99–100; “Tax Measure Offers New Benefits for Hospice Care of Terminally Ill,” New York Times, September 1, 1982, A19. ↩
-
Patricia Berry, “Hospice and Palliative Care: Differences Matter,” International Journal of Palliative Nursing 21, no. 3 (2015): 107. ↩
-
This fact should not obfuscate the problems and inequities that were and are present in hospice as conceived by mission-driven nonprofits. These organizations, the Connecticut Hospice included, often reproduce the systems that are endemic to nonprofits the nation over: whiteness, class hierarchies between the serving and the served, veiled religious intention, administrator burnout, among others. See, for example, Abel, Living in Death’s Shadow, 119–123, for a discussion of the presence of ethnic stereotyping in one of Florence Wald’s patient cases. Rather than replace for-profit hospices with solely nonprofit institutions, I mean to argue for learning from the Connecticut Hospice’s particular approach to spatializing care for care workers. ↩
-
Sharmin Kader, “Development of Hospice Environmental Assessment Protocol (HEAP): A Post Occupancy Evaluation Tool” (dissertation; University of Kansas, Architecture Department, 2016), iii–iv, 284–324. See also Kader and Keith Diaz Moore, “Therapeutic Goals of Hospice Care Environment: A Systematic Literature Review,” in Future of Architectural Research: Architectural Research Centers Consortium 2015, ed. Ajla Aksamija, John Haymaker, and Abbas Aminmansour (Chicago: Perkins + Will, 2015), 492–499, for a summary of the methodology and references used to identify these eleven goals. ↩
-
Paul Eshelman, Rana Sagha Zadeh, Judith Setla, and Ana Krieger, Designing End-of-Life Care Settings to Enhance Quality of Life: Informing the Conversation Among Designers, Users & Stakeholders (Ithaca, NY: Cornell University and Facility Guidelines Institute, 2018). ↩
-
Eshelman et al., Designing End-of-Life Care Settings to Enhance Quality of Life, 28. This sentiment is reiterated in the literature review in Kader, “Development of Hospice Environmental Assessment Protocol (HEAP),” but Kader crucially points out that the “family and staff find privacy more important that patients” (98–99). This very same question—whom, in a hospice setting, do private rooms actually serve?—was at the core of Connecticut Hospice’s contentious decision to leave 61 Burban Drive for 100 Double Beach Road. Hospice, Inc.. founders were quoted in the press to be opposed to the move, insisting that patients prefer shared rooms. Former patrons and patients like Diana Granbery, though, disagreed. Granbery wrote a public rebuttal of the founders’ claims, noting that “not everyone feels the same way about terminal illness and dying. They should have a choice.” See Melinda Tuhus, “A Hospice’s Decision Stirs Opposition,” New York Times, October 31, 1999, CT3; Diana Granbery, “New Hospice Site May Help Program,” New York Times, December 5, 1999, CT8. Though robust studies on this topic are lacking, it seems possible that the Hospice, Inc., founders were fairly on the mark about patient preferences. A 2012 study of seventy-seven patients in a UK inpatient hospice setting found that 56 percent preferred a shared room over a single or didn’t care; 44 percent preferred a private room. However, a whopping 61percent of family members wanted a private room. Mark B. Howard, Stephen Higgins, and Aoife Gleeson, “Hospice Patients’ and Families’ Preference for Shared Versus Single Rooms,” Palliative Medicine 28, no. 1 (January 2014): 94–95. ↩
-
Andrew Julien, “The Old Building Is Modest and Cozy. The New Building Is Grand and Open,” Hartford Courant, December 27, 1999, link. ↩
-
Paul B. Bailey, “Monastery of the Glorious Cross: Existing Conditions Floor Plans,” April 4, 2001, computerized record, Building Department, Branford Town Hall; Associated Press, “Branford Monastery a Haven for Disabled Nuns,” New Haven Register, October 26, 2003, link. ↩
-
See the 2001–2018 computerized records for 61 Burban Drive in the Building Department, Branford Town Hall. ↩
-
61 Burban Drive property listing by the Proto Group, September 4, 2018, link. ↩
-
Greg Bordonaro, “Branford Religious Property Sells for $1.6M,” New Haven Biz, July 8, 2021, link. ↩
-
“Branford Zoning: Jan. 20 ‘Zoom’ Public Hearings to Include Burban Drive Development,” Zip 06, January 14, 2022, link. ↩
-
Many people contributed to the preparation of this study. For their academic, editorial, and intellectual support, I especially thank Kristine Ericson, Anthony Acciavatti, Manu Goswami, Craig Buckley, Jacob R. Moore, Melis Ugurlu, Marisa Cortright, and Andrew Billingsley, along with all the interviewees cited within, who generously shared their time and memories with me. This essay is dedicated to the memory of Dawn Ralston. ↩
Clare Fentress is a designer, writer, and recent graduate of the Yale School of Architecture’s M.Arch. I program, where she received the David Taylor Memorial Prize. The 2022 John Belle Travel Fellow, she previously studied literature at the University of Chicago and is an associate editor at n+1.

